How a Diabetic Retinopathy Specialist Can Help Protect Your Vision
- Steven Cohen

- Apr 23
- 7 min read
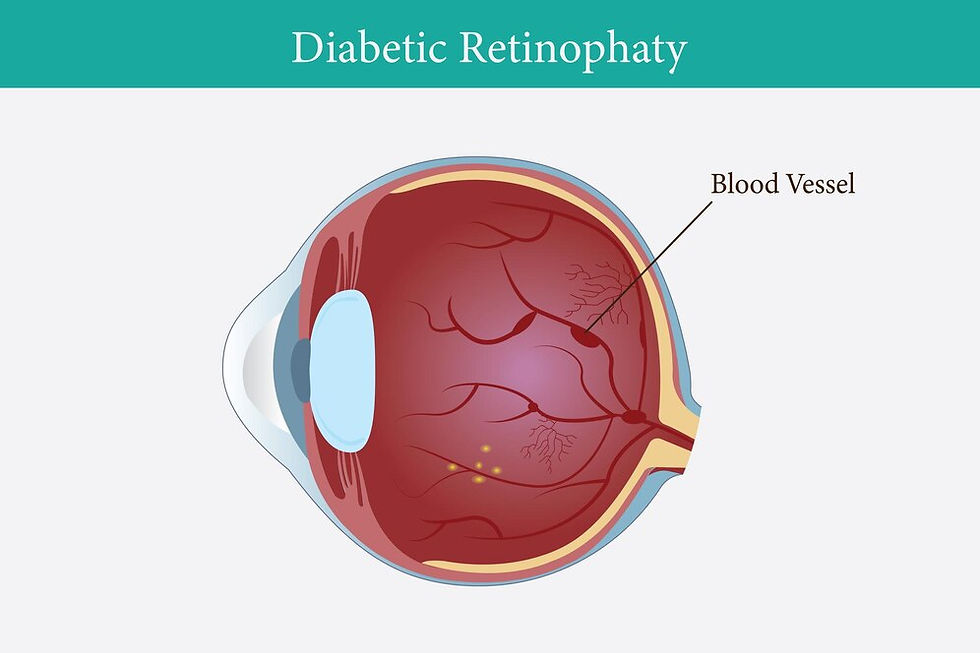
Diabetes is a chronic condition that affects millions of people worldwide, and one of its most serious complications is diabetic retinopathy, a leading cause of blindness in adults. This progressive eye disease damages the blood vessels in the retina, the light-sensitive layer at the back of the eye, potentially leading to vision loss if left untreated. Fortunately, a diabetic retinopathy specialist plays a critical role in diagnosing, treating, and preventing the progression of this condition, helping patients preserve their vision and maintain their quality of life.
In this article, we’ll explore the vital role of a diabetic retinopathy specialist, the nature of diabetic retinopathy, its symptoms and stages, diagnostic methods, treatment options, and preventive measures. By understanding how these specialists work, you can take proactive steps to protect your vision and manage this serious complication of diabetes effectively.
Understanding Diabetic Retinopathy
Diabetic retinopathy is a complication of diabetes that occurs when high blood sugar levels damage the tiny blood vessels in the retina. Over time, these damaged vessels can leak fluid or blood, causing swelling (edema) in the retina or abnormal blood vessel growth, both of which impair vision. The condition typically affects both eyes and progresses through distinct stages, ranging from mild to severe.
Stages of Diabetic Retinopathy
Mild Non-Proliferative Retinopathy (NPDR): This is the earliest stage, characterized by small areas of swelling in the retina’s blood vessels, called microaneurysms. Vision may not be affected at this stage, but early detection is critical.
Moderate NPDR: As the disease progresses, more blood vessels become blocked, leading to reduced blood supply to the retina. This can cause mild vision changes.
Severe NPDR: In this stage, a significant number of blood vessels are blocked, depriving the retina of oxygen and triggering the growth of abnormal blood vessels.
Proliferative Diabetic Retinopathy (PDR): The most advanced stage, PDR involves the growth of fragile, abnormal blood vessels on the retina or optic disc. These vessels can bleed into the vitreous (the gel-like substance in the eye), causing severe vision loss or blindness.
Diabetic retinopathy may also lead to diabetic macular edema (DME), where fluid accumulates in the macula, the part of the retina responsible for sharp central vision. DME can occur at any stage and is a common cause of vision impairment in diabetic patients.
Given the progressive nature of this condition, early intervention by a diabetic retinopathy specialist is essential to prevent irreversible damage.
The Role of a Diabetic Retinopathy Specialist
A diabetic retinopathy specialist is typically a retina specialist or an ophthalmologist with advanced training in diagnosing and treating retinal disorders, particularly those caused by diabetes. These specialists have expertise in the latest diagnostic tools, medical treatments, and surgical procedures to manage diabetic retinopathy and its complications.
Why See a Diabetic Retinopathy Specialist?
While general ophthalmologists can perform routine eye exams, a diabetic retinopathy specialist offers specialized care tailored to the unique needs of diabetic patients. Here are some key reasons to consult a specialist:
Expert Diagnosis: Specialists use advanced imaging technologies to detect early signs of diabetic retinopathy, often before symptoms appear.
Personalized Treatment Plans: They create customized treatment strategies based on the stage of the disease, the patient’s overall health, and their specific vision needs.
Access to Cutting-Edge Treatments: Specialists are trained in the latest therapies, including laser treatments, anti-VEGF injections, and vitreoretinal surgery.
Preventive Care: They provide guidance on managing diabetes and lifestyle factors to slow disease progression and protect vision.
Management of Complications: Specialists can address complications like DME, retinal detachment, or vitreous hemorrhage, which require advanced expertise.
By working closely with a diabetic retinopathy specialist, patients can receive comprehensive care that addresses both immediate concerns and long-term vision health.
Symptoms of Diabetic Retinopathy
One of the challenges of diabetic retinopathy is that it often develops without noticeable symptoms in its early stages. As the disease progresses, patients may experience:
Blurred or fluctuating vision
Dark spots or floaters in the field of vision
Difficulty seeing at night
Colors appearing faded or washed out
A shadow or curtain across part of the visual field
Sudden vision loss (in advanced cases)
Because symptoms may not appear until significant damage has occurred, regular eye exams with a diabetic retinopathy specialist are crucial for early detection and intervention.
Diagnostic Techniques Used by Specialists
A diabetic retinopathy specialist employs a range of sophisticated diagnostic tools to assess the health of the retina and detect signs of diabetic retinopathy. These include:
1. Dilated Eye Exam
During a dilated eye exam, the specialist uses eye drops to widen the pupils, allowing a clear view of the retina and optic nerve. This exam helps identify microaneurysms, hemorrhages, or abnormal blood vessels.
2. Fundus Photography
This involves taking high-resolution images of the retina to document the presence and extent of diabetic retinopathy. These images serve as a baseline for monitoring disease progression.
3. Optical Coherence Tomography (OCT)
OCT is a non-invasive imaging technique that provides detailed cross-sectional images of the retina. It is particularly useful for detecting macular edema and assessing the thickness of the retina.
4. Fluorescein Angiography
In this procedure, a fluorescent dye is injected into the bloodstream, and photographs are taken as the dye circulates through the retinal blood vessels. This test highlights leaking or blocked vessels and abnormal blood vessel growth.
5. OCT Angiography
A newer, non-invasive alternative to fluorescein angiography, OCT angiography visualizes blood flow in the retina and choroid without the need for dye. It is increasingly used for precise diagnosis.
These diagnostic tools enable a diabetic retinopathy specialist to accurately stage the disease and develop an effective treatment plan.
Treatment Options for Diabetic Retinopathy
The treatment approach for diabetic retinopathy depends on the stage of the disease, the presence of complications like DME, and the patient’s overall health. A diabetic retinopathy specialist may recommend one or more of the following treatments:
1. Monitoring and Lifestyle Changes
For mild NPDR, the specialist may recommend close monitoring through regular eye exams without immediate treatment. Managing blood sugar, blood pressure, and cholesterol levels is critical to slow disease progression. The specialist may collaborate with the patient’s primary care physician or endocrinologist to optimize diabetes management.
2. Anti-VEGF Injections
Anti-vascular endothelial growth factor (VEGF) injections, such as ranibizumab (Lucentis), aflibercept (Eylea), or bevacizumab (Avastin), are commonly used to treat DME and PDR. These medications reduce abnormal blood vessel growth and leakage, improving vision in many cases. Injections are administered directly into the eye under local anesthesia and may be required monthly or as needed.
3. Laser Photocoagulation
Laser treatment, also known as panretinal photocoagulation or focal laser treatment, is used to seal leaking blood vessels or shrink abnormal ones. This procedure can stabilize vision but may not restore lost vision. It is often used for severe NPDR or PDR.
4. Corticosteroid Implants
For patients with DME who do not respond to anti-VEGF therapy, corticosteroid implants like dexamethasone (Ozurdex) or fluocinolone acetonide (Iluvien) may be used to reduce inflammation and swelling in the macula.
5. Vitrectomy
In advanced cases of PDR, where vitreous hemorrhage or retinal detachment occurs, a vitrectomy may be necessary. This surgical procedure removes blood and scar tissue from the vitreous, restoring clear vision. A diabetic retinopathy specialist with surgical expertise performs this delicate operation.
6. Emerging Therapies
Research is ongoing into new treatments, such as gene therapies and sustained-release drug delivery systems, which may offer additional options in the future. A diabetic retinopathy specialist stays updated on these advancements to provide cutting-edge care.
Preventive Measures to Protect Your Vision
While a diabetic retinopathy specialist plays a pivotal role in managing diabetic retinopathy, patients can take proactive steps to protect their vision. Here are some key preventive measures:
1. Control Blood Sugar Levels
Maintaining blood glucose within target ranges reduces the risk of retinal damage. Work with your healthcare team to monitor HbA1c levels and follow a diabetes-friendly diet.
2. Manage Blood Pressure and Cholesterol
High blood pressure and cholesterol can exacerbate diabetic retinopathy. Regular monitoring and medications, if needed, can help keep these under control.
3. Schedule Regular Eye Exams
Annual or biannual eye exams with a diabetic retinopathy specialist are essential for early detection, even if you have no symptoms. Early intervention can prevent vision loss.
4. Quit Smoking
Smoking worsens blood vessel damage and increases the risk of diabetic retinopathy. Quitting smoking can improve overall eye health.
5. Stay Active
Regular physical activity improves blood circulation and helps manage diabetes, reducing the risk of complications like diabetic retinopathy.
6. Follow Your Specialist’s Recommendations
Adhere to the treatment and monitoring plan outlined by your diabetic retinopathy specialist. Attend all follow-up appointments to track your condition.
The Importance of Early Intervention
The earlier diabetic retinopathy is detected, the better the chances of preserving vision. A diabetic retinopathy specialist can identify subtle changes in the retina before symptoms arise, allowing for timely intervention. Delaying treatment can lead to irreversible vision loss, making regular screenings a priority for all diabetic patients.
Choosing the Right Diabetic Retinopathy Specialist
When selecting a diabetic retinopathy specialist, consider the following factors:
Credentials and Experience: Look for a board-certified ophthalmologist with fellowship training in retinal disorders.
Access to Advanced Technology: Ensure the specialist’s practice is equipped with state-of-the-art diagnostic and treatment tools.
Patient-Centered Care: Choose a specialist who communicates clearly, answers questions, and involves you in decision-making.
Collaboration with Your Healthcare Team: The specialist should work with your primary care physician or endocrinologist to provide holistic care.
You can find a qualified diabetic retinopathy specialist through referrals from your primary care doctor, diabetes educator, or organizations like the American Academy of Ophthalmology.
Living with Diabetic Retinopathy
A diagnosis of diabetic retinopathy can be overwhelming, but with the right care, many patients maintain good vision and lead fulfilling lives. A diabetic retinopathy specialist not only provides medical treatment but also offers support and education to help you manage your condition. Joining a diabetes support group or working with a low-vision specialist can also enhance your quality of life if vision loss occurs.
Conclusion
Diabetic retinopathy is a serious complication of diabetes, but with the expertise of a diabetic retinopathy specialist, it is possible to protect your vision and prevent severe outcomes. Through early detection, advanced treatments, and proactive management of diabetes, these specialists play an indispensable role in safeguarding your eye health. By scheduling regular eye exams, following your specialist’s recommendations, and adopting a healthy lifestyle, you can take control of your vision and reduce the impact of diabetic retinopathy.
If you have diabetes, don’t wait for symptoms to appear—consult a diabetic retinopathy specialist today to ensure your eyes remain healthy for years to come. Your vision is worth protecting, and with the right care, you can continue to see the world clearly.



Comments